Coughing and Chest Pain: Possible Triggers and Care Considerations
Coughing paired with chest pain can feel alarming because it involves two symptoms linked to both minor illnesses and medical emergencies. In the United States, the safest approach is to consider the pattern, severity, and any accompanying warning signs, and to seek urgent evaluation when the cause is unclear or symptoms escalate.
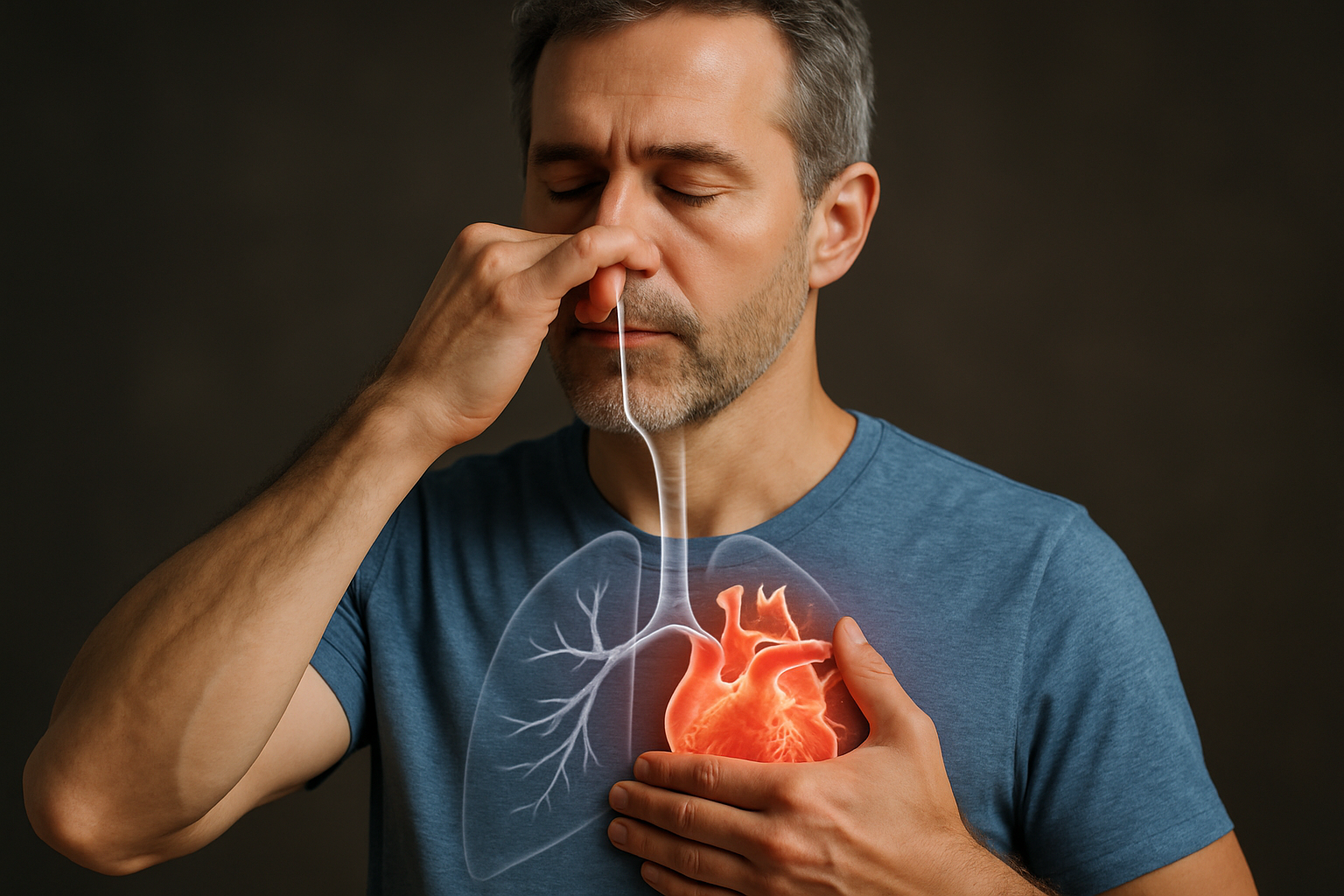
Chest discomfort with a cough is often caused by irritation or strain in the airways and chest wall, but it can also reflect problems involving the heart, lungs, or blood vessels. Because these conditions can overlap in how they feel, focusing on practical clues—how the pain behaves, what triggers it, and what else you notice—can help guide safer decisions about care.
Coughing and chest pain: common triggers
One of the most common explanations is inflammation from a respiratory infection. Viral bronchitis, influenza, COVID-19, or pneumonia can irritate the lining of the airways, leading to frequent coughing and soreness or burning in the chest. Pain may worsen with deep breaths, laughter, or repeated coughing fits, and may come with fever, fatigue, or shortness of breath.
Muscle strain is another frequent cause. Vigorous or prolonged coughing can strain the intercostal muscles between the ribs or irritate cartilage where ribs attach to the breastbone (costochondritis). This tends to produce localized tenderness that is reproducible—meaning pressing on a specific spot or moving the torso can make the pain noticeably worse.
Acid reflux can also link cough and chest discomfort. Gastroesophageal reflux disease (GERD) may trigger a chronic cough (especially at night or after meals) and cause a burning sensation behind the breastbone. Some people also develop laryngopharyngeal reflux, where irritation higher in the throat contributes to coughing, throat clearing, and chest tightness.
Some triggers are less common but more urgent. A pulmonary embolism (a blood clot in the lungs) can cause sudden chest pain that may worsen with breathing, along with shortness of breath, a fast heart rate, lightheadedness, or coughing up blood. Pleurisy (inflammation of the lung lining) can cause sharp, stabbing pain with breathing or coughing and may occur with infections or autoimmune conditions.
Heart-related conditions can overlap with cough-associated chest symptoms. Heart failure can cause fluid buildup in the lungs leading to cough (sometimes worse when lying down) and chest pressure or tightness. Reduced blood flow to the heart muscle (angina) or a heart attack may present as pressure, squeezing, heaviness, or pain that can radiate to the arm, jaw, neck, or back; some people also notice nausea, sweating, or unusual fatigue. While coughing itself is not a typical “trigger” for a heart attack, chest discomfort that appears during exertion, stress, or at rest with concerning features deserves immediate attention.
Coughing and chest pain symptoms to watch
To interpret coughing and chest pain symptoms, it helps to note the character of pain and the context. Sharp pain that worsens with deep breaths or coughing can point toward pleuritic causes such as pneumonia, pleurisy, or a pulmonary embolism. Pain that is reproducible with pressing on the chest wall or twisting may fit muscle strain or costochondritis.
Pressure-like, squeezing, or heavy chest discomfort—especially if it is not clearly linked to a specific sore spot—raises more concern for cardiac causes. This is particularly important when the discomfort is paired with shortness of breath, sweating, nausea, faintness, or pain radiating to the jaw, arm, shoulder, neck, or back. Not everyone experiences “classic” chest pain; some people, including women, older adults, and people with diabetes, may have subtler symptoms such as fatigue, breathlessness, indigestion-like discomfort, or nausea.
Also consider the timing and triggers. A cough and chest tightness that flare with allergens, cold air, or exercise may suggest asthma. Wheezing, a whistling sound when breathing out, or a history of allergies can support that pattern. If symptoms follow a new medication, note that some drugs (such as ACE inhibitors used for blood pressure) can cause a persistent dry cough, though chest pain is less typical and should still be evaluated if present.
Red-flag features in coughing and chest pain symptoms include sudden onset; severe intensity; worsening shortness of breath; confusion; bluish lips; coughing up blood; new leg swelling or pain (a possible clot source); fainting; or chest pressure that lasts more than a few minutes or returns. In the United States, call 911 for these signs or if you suspect a heart attack—driving yourself can delay care.
Chest pain management and safer next steps
Chest pain management starts with avoiding assumptions. Until a serious cause is ruled out, it is safer to limit exertion and monitor symptoms closely. If the pain is mild, clearly linked to coughing or a tender chest wall area, and you have no warning signs, supportive measures may help while you arrange timely medical assessment.
For cough-related soreness, staying hydrated, using humidified air, and treating the underlying cough trigger can reduce strain on the chest wall. If you use over-the-counter pain relievers, follow label directions and consider your medical history: NSAIDs (like ibuprofen or naproxen) may not be appropriate for some people with kidney disease, stomach ulcers, blood-thinner use, or certain heart conditions. If reflux seems involved, smaller meals, avoiding late-night eating, and limiting trigger foods (such as alcohol, spicy foods, or high-fat meals) can reduce irritation that may perpetuate coughing.
Clinical evaluation is often the key step when symptoms are new, persistent, or unclear. A clinician may assess vital signs, listen to heart and lungs, check oxygen levels, and review risk factors such as smoking history, asthma/COPD, recent surgery or travel, pregnancy/postpartum status, clotting history, and family history of heart disease. Depending on findings, testing may include an electrocardiogram (ECG), blood tests (such as troponin for heart muscle injury), chest X-ray, viral testing, or imaging such as CT when a clot or other urgent condition is suspected.
If you have known heart disease risk factors—high blood pressure, high cholesterol, diabetes, smoking, kidney disease, or a strong family history—take any unexplained chest pressure seriously, even if you also have a cough. Respiratory infections can increase cardiac strain through fever, dehydration, and inflammation, which is one reason heart symptoms sometimes emerge during or after an illness.
This article is for informational purposes only and should not be considered medical advice. Please consult a qualified healthcare professional for personalized guidance and treatment.
Coughing with chest pain is often explained by infections, reflux, asthma, or chest-wall strain, but it can also signal urgent lung or heart conditions. Tracking the quality of pain, its triggers, and associated symptoms helps clarify risk, yet the safest approach is prompt evaluation whenever symptoms are severe, sudden, persistent, or accompanied by warning signs.




