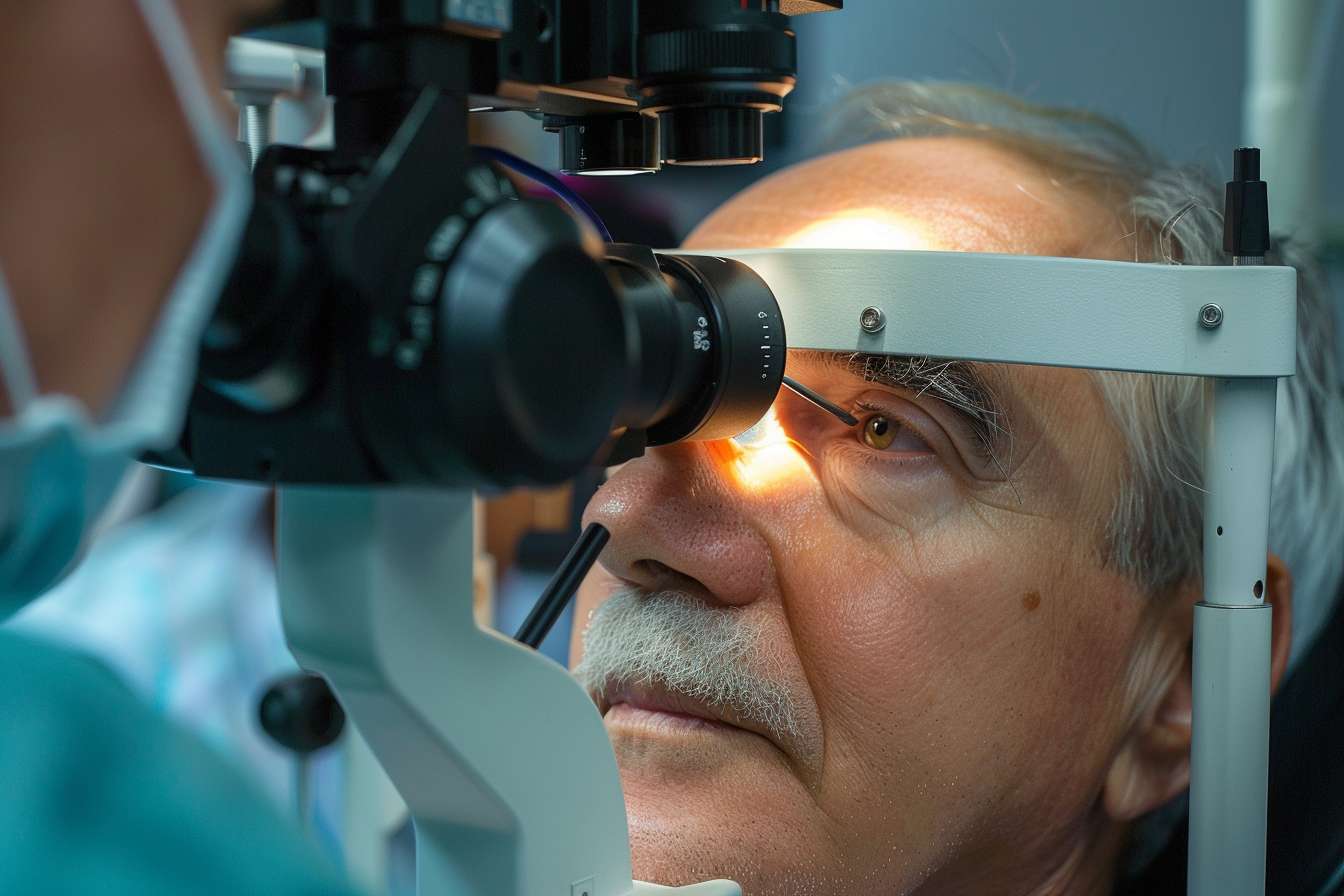
Cataract Surgery for Seniors: What to Expect Before and After
Cataracts are a common age-related condition that affects millions of seniors across the United States, gradually clouding vision and impacting daily activities. As the lens of the eye becomes opaque over time, simple tasks like reading, driving, or recognizing faces can become increasingly difficult. Fortunately, cataract surgery is a well-established, safe procedure that restores clarity and improves quality of life for older adults. Understanding what happens before, during, and after the procedure can help seniors and their families approach this common surgery with confidence and realistic expectations.
Cataracts develop when proteins in the eye’s natural lens break down and clump together, causing cloudiness that interferes with vision. This process is a natural part of aging, and by age 80, more than half of Americans either have cataracts or have undergone surgery to remove them. While cataracts cannot be reversed with medication or lifestyle changes, surgical intervention offers a highly effective solution. The procedure involves removing the clouded lens and replacing it with an artificial intraocular lens, restoring clear vision in most cases.
What Is Cataract Surgery for Seniors?
Cataract surgery is an outpatient procedure designed to remove the clouded natural lens of the eye and replace it with a clear artificial lens. For seniors, this surgery is often recommended when cataracts begin to interfere with daily activities such as reading, driving, or watching television. The decision to proceed with surgery is typically made in consultation with an ophthalmologist, who evaluates the severity of the cataract and the impact on the patient’s quality of life. Most seniors experience significant improvement in vision following the procedure, which is performed under local anesthesia and takes approximately 15 to 30 minutes per eye.
Types of Cataract Surgery Available
There are two primary surgical techniques used to treat cataracts in seniors. Phacoemulsification, the most common method, involves making a small incision in the cornea and using ultrasound waves to break up the clouded lens into tiny fragments, which are then gently suctioned out. This minimally invasive approach allows for faster healing and fewer complications. Extracapsular cataract extraction is an alternative technique used in more advanced cases where the cataract is too dense for phacoemulsification. This method requires a larger incision to remove the lens in one piece. Both procedures conclude with the insertion of an artificial intraocular lens to restore focusing ability.
Cataract Surgery Options and Lens Choices
Seniors undergoing cataract surgery have several lens options to consider, each offering different benefits. Monofocal lenses are the standard choice, providing clear vision at a single distance, typically for far vision, though reading glasses may still be needed. Multifocal lenses offer the advantage of clear vision at multiple distances, reducing dependence on glasses for both near and far tasks. Toric lenses are designed specifically for patients with astigmatism, correcting both the cataract and the irregular curvature of the cornea. The choice of lens depends on individual lifestyle needs, visual goals, and budget considerations, as premium lenses may involve additional out-of-pocket costs.
What to Expect Before the Procedure
Before cataract surgery, seniors undergo a comprehensive eye examination to measure the eye and determine the appropriate lens power. This preoperative assessment includes tests to evaluate overall eye health and identify any other conditions that might affect surgery outcomes. Patients are typically instructed to avoid eating or drinking for several hours before the procedure and may be prescribed antibiotic eye drops to reduce the risk of infection. On the day of surgery, patients should arrange for transportation, as they will not be able to drive immediately afterward. The surgical team will explain the process, answer questions, and ensure the patient feels comfortable and informed.
Recovery and What to Expect After Surgery
Recovery from cataract surgery is generally quick, with most seniors noticing improved vision within a few days. Immediately after the procedure, the eye may feel scratchy or slightly uncomfortable, and vision may be blurry as the eye adjusts to the new lens. Patients are given protective eyewear and prescribed eye drops to prevent infection and reduce inflammation. It is important to avoid rubbing the eye, engaging in strenuous activities, or exposing the eye to water for at least a week. Follow-up appointments allow the ophthalmologist to monitor healing and address any concerns. Most seniors return to normal activities within a few days, though complete healing can take several weeks.
Potential Risks and Considerations for Seniors
While cataract surgery is considered very safe, seniors should be aware of potential risks and complications. These can include infection, bleeding, inflammation, or increased eye pressure. In rare cases, the artificial lens may shift position, or a secondary cataract may develop on the membrane surrounding the lens, requiring a simple laser procedure to correct. Seniors with other eye conditions, such as glaucoma or macular degeneration, may experience less dramatic vision improvement. Discussing medical history and any concerns with the ophthalmologist before surgery helps ensure realistic expectations and optimal outcomes.
Cost Estimation and Provider Comparison
The cost of cataract surgery for seniors in the United States varies depending on the type of procedure, lens choice, and geographic location. Medicare typically covers standard cataract surgery with a monofocal lens, though patients may face copayments or deductibles. Premium lens options, such as multifocal or toric lenses, often involve additional out-of-pocket expenses. Below is a general comparison of typical costs and providers:
| Provider Type | Procedure Type | Estimated Cost Range |
|---|---|---|
| Hospital-Based Surgery Center | Phacoemulsification with Monofocal Lens | $3,000 - $5,000 per eye |
| Ambulatory Surgery Center | Phacoemulsification with Multifocal Lens | $4,500 - $7,000 per eye |
| Private Ophthalmology Practice | Extracapsular Extraction with Monofocal Lens | $3,500 - $6,000 per eye |
| Academic Medical Center | Phacoemulsification with Toric Lens | $4,000 - $6,500 per eye |
Prices, rates, or cost estimates mentioned in this article are based on the latest available information but may change over time. Independent research is advised before making financial decisions.
This article is for informational purposes only and should not be considered medical advice. Please consult a qualified healthcare professional for personalized guidance and treatment.
Cataract surgery remains one of the most successful and commonly performed procedures for seniors, offering a pathway to restored vision and improved independence. By understanding the process, options, and recovery expectations, older adults can approach this life-enhancing surgery with confidence and peace of mind.